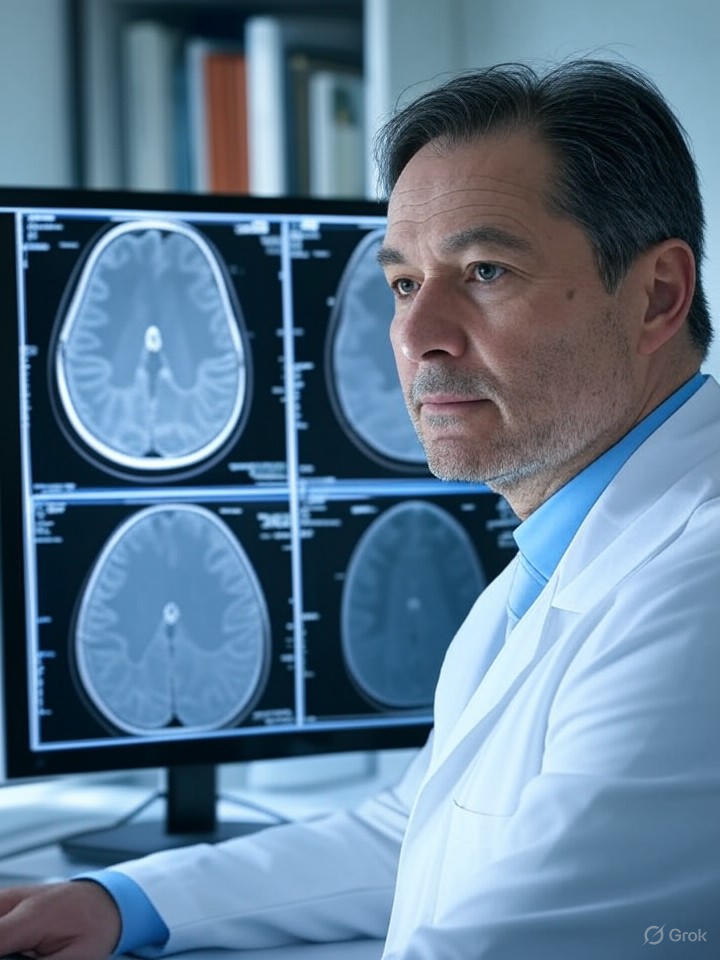
Recent advancements in artificial intelligence are significantly transforming cancer diagnosis, achieving an impressive accuracy improvement of up to 45%. This development is particularly crucial as early detection remains a vital factor in successful cancer treatment. According to a report from MSN, AI systems are increasingly being integrated into clinical practice, where they assist medical professionals in identifying subtle anomalies in medical imaging that may go unnoticed by the human eye.
The utilization of AI in oncology stems from sophisticated machine learning algorithms that have been trained on extensive datasets, including millions of annotated scans and patient records. Researchers at Harvard Medical School have developed tools that analyze features from a tumor’s microenvironment to predict patient responses to various therapies. This innovation allows for tailored treatment plans that are more aligned with individual patient needs.
The Mechanics Behind AI Diagnostics
Central to the functionality of these AI systems are deep learning models designed to process imaging data from MRIs, CT scans, and biopsies. A study published in the PMC highlights how these technologies effectively facilitate early detection and accurate diagnoses, addressing cancer as a leading global cause of death. By cross-referencing historical data with real-time inputs, AI tools significantly reduce both false positives and negatives, contributing to the reported 45% enhancement in diagnostic precision.
This advancement is especially important in resource-limited settings, where access to experienced radiologists may be limited. Beyond detection, AI is also being employed to predict patient survival rates and treatment outcomes. The Cancer Research Institute notes that AI is revolutionizing cancer care by analyzing genetic markers alongside imaging results, thereby enabling oncologists to customize therapies such as immunotherapy or chemotherapy based on AI-generated insights.
Challenges and Ethical Considerations
Despite the promising capabilities of AI in cancer care, its widespread adoption faces several challenges. Concerns regarding data privacy, algorithmic bias, and the necessity for thorough validation remain prominent. An article from the NCI raises questions about the readiness of AI for routine clinical use, cautioning that biased training data could worsen disparities in healthcare outcomes, particularly among underrepresented populations.
Furthermore, integrating AI into existing medical workflows demands significant investment in training and infrastructure. This point is underscored by insights from Winship Magazine, which emphasize the importance of collaboration between technology companies and medical institutions. For instance, Google has initiated health projects focused on developing AI systems for breast cancer detection in partnership with clinicians. These collaborations aim to ensure that AI tools are not only precise but also equitable and transparent, fostering trust among healthcare providers and patients alike.
Looking ahead, the convergence of AI with emerging technologies such as genomics and wearable sensors could further enhance diagnostic capabilities. A recent report from Stanford Medicine discusses a groundbreaking AI tool that integrates medical images with textual data to predict patient prognoses. This innovative approach signals the onset of a new era in precision oncology, with the potential to streamline clinical trials and accelerate drug development.
As AI continues to reshape cancer diagnosis, stakeholders from biotech firms to regulatory bodies are closely monitoring its evolution. The reported 45% accuracy increase may represent just the beginning of a transformative journey in cancer care. Industry experts project that within the next decade, AI could become an essential ally in combating this pervasive disease, ultimately enhancing patient outcomes on a global scale.