A former office manager of a home care agency in Montgomery County, Pennsylvania, has been sentenced to prison for her involvement in a substantial Medicaid fraud scheme. Barbara Thomas, aged 46, was sentenced to serve between 9 to 23 months in state prison, followed by four years of probation, after admitting guilt to felony counts of Medicaid fraud, theft by deception, and involvement in corrupt organizations.
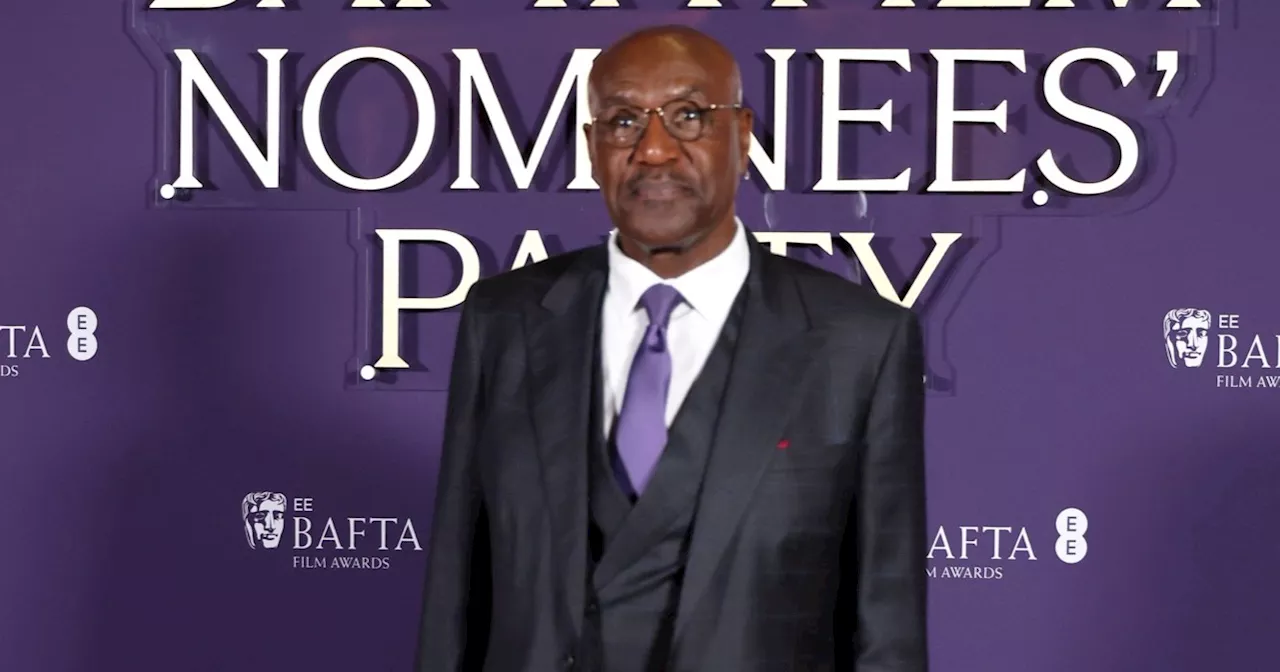
Attorney General Dave Sunday announced the sentencing this week, emphasizing the impact of the crime on taxpayers and vulnerable individuals relying on Medicaid services. Thomas is also required to pay $1.39 million in restitution, jointly with her co-defendants, to help recover losses linked to the fraudulent activities.
Details of the Fraudulent Scheme
Investigators revealed that Thomas held dual roles as both office manager and case manager at ComfortZone Home Health Care from 2020 to 2023. During this time, the agency submitted numerous claims to Medicaid for personal care services that were not actually provided. Authorities indicated that Thomas was integral to the daily operations of ComfortZone and played a significant role in facilitating fraudulent billing practices, which led to improper payments totaling nearly $1.76 million.
“This defendant had her hands in the day-to-day operations and was integrally involved in the advancement of a multi-year scheme that stole from taxpayers and defrauded a system designed to help vulnerable Pennsylvanians,” said Attorney General Sunday. He highlighted the effectiveness of the Medicaid Fraud Control Section, noting its national leadership in combating fraud and abuse within the system.
Broader Implications and Ongoing Investigations
The charges against Thomas were part of a comprehensive two-year investigation conducted by the Pennsylvania Office of Attorney General’s Medicaid Fraud Control Section and the FBI, supported by findings from the Fiftieth Statewide Investigating Grand Jury. Prosecutors stated that the fraud was orchestrated by ComfortZone’s owner, Stephanie Mobley, who was authorized as a Medicaid provider for personal assistance services.
Mobley, along with 20 other alleged co-conspirators, has been charged with submitting false claims for care that was never delivered. To date, 18 individuals associated with the conspiracy have pleaded guilty, including Mobley, who is currently awaiting sentencing. Legal proceedings against three remaining defendants are still in progress, with the cases being managed by Senior Deputy Attorney General Benjamin McKenna.
Under legal statutes, all defendants are presumed innocent until proven guilty in a court of law. This case sheds light on the ongoing challenges in safeguarding public funds meant for essential services, underscoring the importance of vigilance and accountability in the healthcare system.