The increasing strain on healthcare systems in the United States and the United Kingdom has led to significant operational challenges, particularly in surgical departments. U.S. hospitals are reducing surgical schedules due to staffing shortages, while the NHS reports over seven million patients waiting for treatment in England. The result is a troubling situation for patients, who face longer wait times and deteriorating health conditions, and for staff, who endure unpredictable workloads and stress.
These operational delays carry substantial financial implications, costing U.S. hospital systems an estimated $32.7 billion annually. Operating rooms (ORs) are notably affected, as they are the most resource-intensive areas within hospitals. They account for as much as 40% of total hospital costs, yet inefficiencies lead to frequent last-minute cancellations and delays. Surgical teams often spend excessive time managing scheduling conflicts, further exacerbating the crisis.
According to a recent survey of OR leaders, many reported that colleagues left their positions in the past two years primarily due to the poor work-life balance created by extended hours and job-related stress. As surgical staff face increasing pressures, the quality of patient care is inevitably compromised.
Transforming Surgical Efficiency Through Technology
The challenges confronting healthcare are chronic and systemic, necessitating immediate action. Digitizing the operating room presents a viable pathway to enhance operational efficiency. Technologies such as real-time data visibility, artificial intelligence, and automation can address core issues, including unreliable data and scheduling complexity. Platforms like Proximie offer solutions that enable surgical teams to foresee potential issues, streamline their schedules, and maintain the flow of procedures.
Data-driven insights can reveal significant opportunities to reduce downtime between surgeries and optimize operating room utilization. For example, a major healthcare provider in the U.S. discovered that approximately 24% of total OR time—averaging 38 minutes per procedure—could be optimized outside of incision time. Capturing this potential equates to an estimated $90 million in annual savings, which could be reinvested into staffing, processes, and equipment, ultimately fostering a more resilient surgical environment.
The healthcare sector is facing a pressing workforce crisis. Projections indicate a shortage of 30,000 surgeons in the U.S. by 2034, compounded by nurse staffing levels remaining below pre-pandemic figures. In the U.K., over three million patients have already exceeded the NHS’s 18-week target for elective surgeries. Furthermore, nearly one in five healthcare workers globally has left their positions since 2020.
Addressing this challenge requires more than just recruiting additional staff. The working environment for existing personnel must become more manageable. Predictability in daily operations is essential not only for efficiency but also for staff wellbeing. When surgical teams can anticipate their schedules and avoid delays, it enhances job satisfaction, reduces turnover, and ultimately improves patient care.
Building a Sustainable Future for Surgery
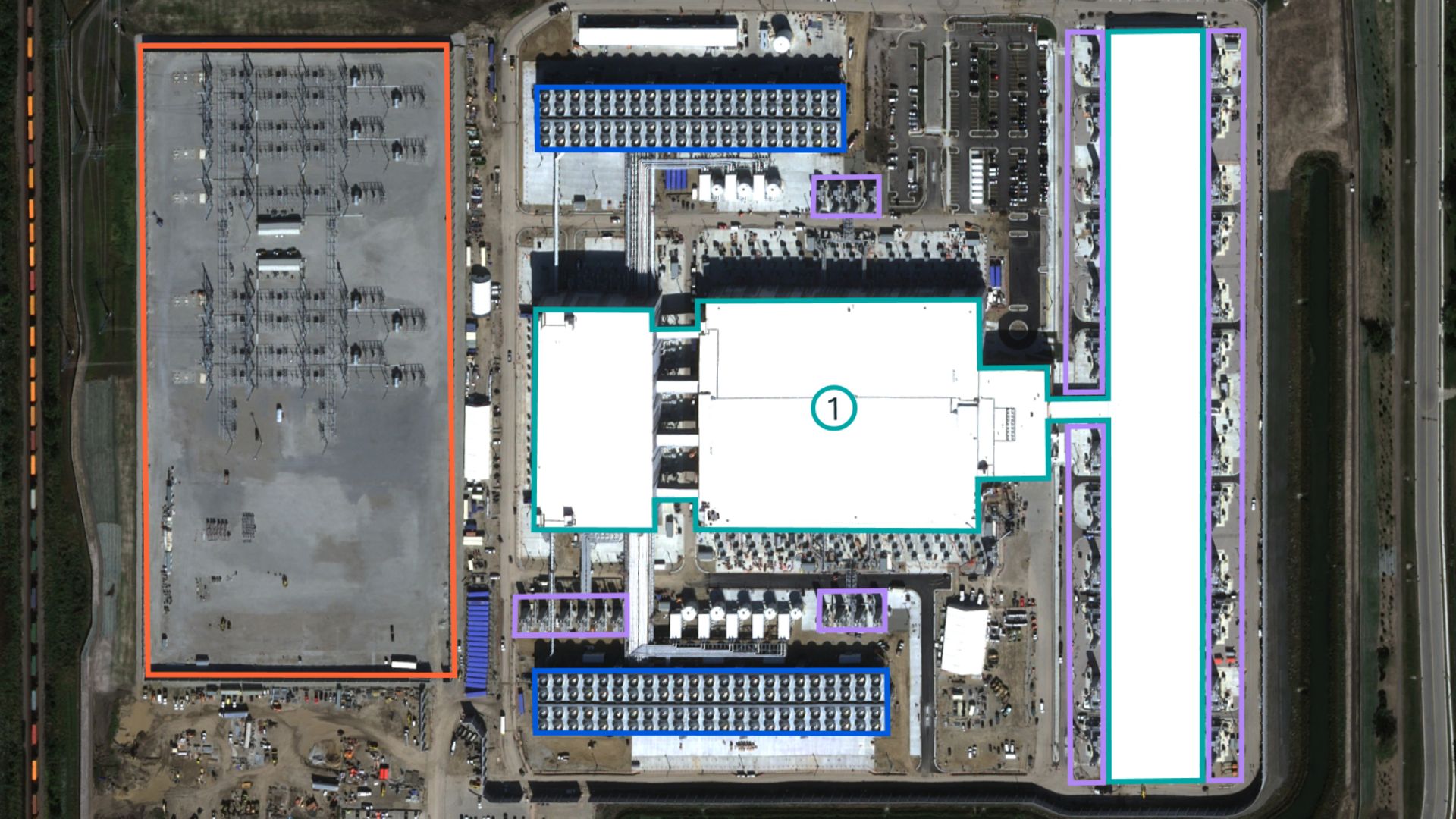
The key to elevating OR efficiency lies in tackling inefficiencies at their source. Many operating rooms still depend on retrospective data, lacking real-time insights into delays and operational bottlenecks. Without accurate, live information, inefficiencies continue unchecked, leading to increased workloads and higher burnout rates among staff.
In contrast, digitized OR environments that provide immediate, detailed data empower clinical teams to precisely monitor time usage, identify bottlenecks, and seize optimization opportunities. Transitioning from reactive to proactive management can foster a safer, more predictable surgical environment, essential for clinician success.
Dr. Nadine Hachach-Haram, founder and CEO of Proximie, emphasizes the importance of innovation in improving surgical care. A practicing NHS surgeon and clinical entrepreneur, Dr. Hachach-Haram’s vision for a digitally connected global surgical workforce has garnered international recognition. She was awarded the British Empire Medal and selected to participate in the Endeavor entrepreneur programme, reflecting her commitment to advancing healthcare accessibility and education.
As the healthcare sector reaches a critical juncture, the choice is clear: continue with outdated methods that threaten workforce stability or embrace smarter systems that empower clinicians to deliver efficient and effective care. The future of surgery hinges on these transformative changes, and the time to act is now.