BOSTON — A new study suggests a more accurate method for assessing health risks, challenging the traditional reliance on Body Mass Index (BMI) as a measure of weight-related health issues.
Breaking: New Approach to Measuring Weight
Health professionals have long used BMI as a quick screening tool to identify patients at risk of health problems due to weight. However, BMI’s calculation of health risk based solely on height and weight has been criticized for its inaccuracies. According to the Harvard T.H. Chan School of Public Health, BMI can overestimate risks for individuals with muscular builds and underestimate concerns for older adults or those with muscle loss.
Immediate Impact
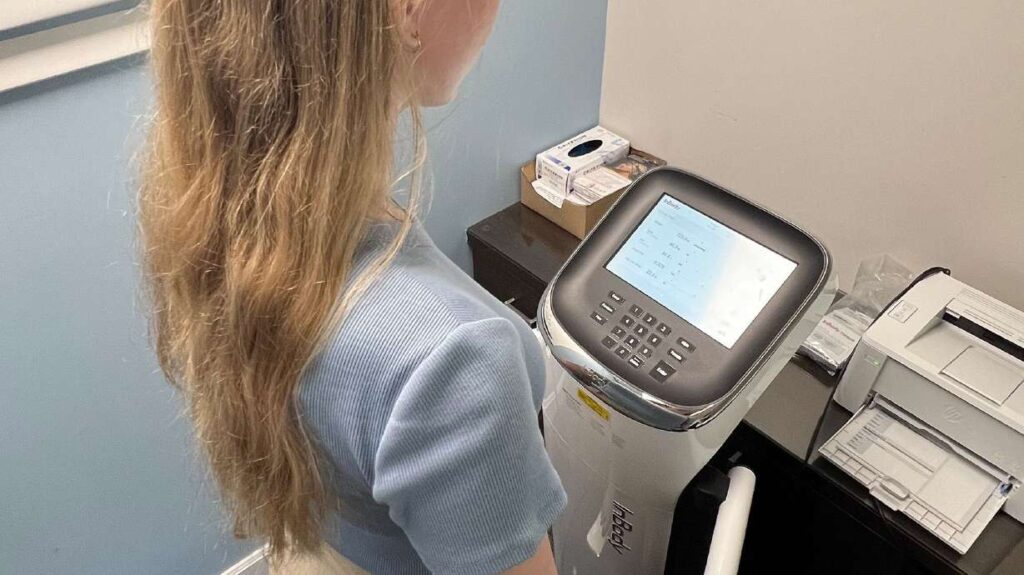
Authors of the new study propose bioelectrical impedance analysis (BIA) as a superior method for predicting future health issues. BIA measures body fat percentage, lean muscle mass, and water weight using undetectable electric currents.
“We found body-fat percentage to be a stronger predictor of 15-year mortality risk in adults between the ages of 20 and 49 than BMI,” said Arch Mainous III, lead author of the study published in the journal Annals of Family Medicine.
Key Details Emerge
The study highlights that individuals with high body fat, as measured by BIA, were 262% more likely to die from heart disease than those with a healthy body fat percentage. This contrasts with BMI, which did not flag any risk in younger populations typically not considered at high risk for heart disease.
“Think of the interventions we can do to keep them healthy when we know this early. I think it’s a game-changer for how we should look at body composition,” said Dr. Frank Orlando, a clinical associate professor at University of Florida Health.
Industry Response
While BMI is commonly used due to its simplicity and low cost, the study suggests a shift towards more direct measurements like BIA. Mainous noted that while DEXA scans are the gold standard, their high cost and limited availability make BMI a fallback option for many health professionals. BIA, however, offers a more accessible and accurate alternative.
“We found the newer versions of bioelectrical impedance are pretty accurate, giving some valid and reliable results,” Orlando said.
By the Numbers
- 78% more likely to die from any cause for those with high body fat measured by BIA.
- 262% increased risk of heart disease-related death with high body fat.
What Comes Next
The study analyzed data from 4,252 participants in the National Health and Nutrition Examination Survey (NHANES) from 1999 to 2004, comparing results with the National Death Index through 2019. The findings suggest a reevaluation of how health risks are assessed, advocating for the inclusion of BIA in routine health assessments.
Expert Analysis
Dr. Andrew Freeman, director of cardiovascular prevention and wellness at National Jewish Health in Denver, cautioned against relying solely on at-home BIA products due to their variability based on hydration levels. However, he acknowledged the potential of clinic-based BIA machines to provide more precise measurements.
Background Context
BMI is calculated by dividing weight by the square of height, categorizing individuals into underweight, healthy weight, overweight, and various obesity classes. While effective at a population level, it fails to account for individual variations in body composition, such as muscle and fat distribution.
“Those people are more likely to have nonalcoholic fatty liver disease, more likely to have elevated glucose, more likely to have elevated blood pressure, and more likely to have inflammation in general,” Mainous said.
Regional Implications
The findings could influence health guidelines and policies, particularly in regions where obesity and related health issues are prevalent. By adopting BIA, healthcare providers could better identify at-risk individuals and tailor interventions to improve health outcomes.
Timeline of Events
- 1999-2004: Data collected from NHANES participants.
- 2019: Analysis compared with National Death Index.
- 2023: Study published in Annals of Family Medicine.
As the medical community continues to explore more accurate methods of assessing health risks, the integration of BIA into standard practice may represent a significant advancement in preventative healthcare.







