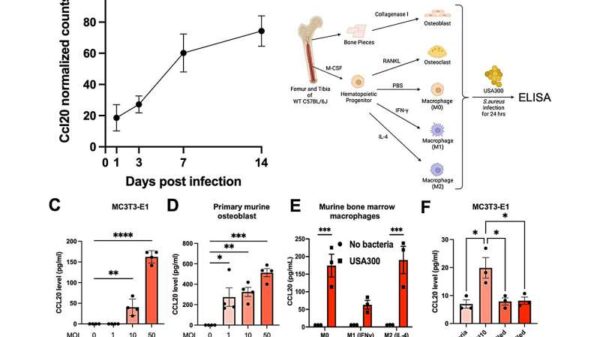
Research from the University of Rochester Medical Center has identified a small protein that could revolutionize the way bone infections are diagnosed and treated. The protein, known as CCL20, may serve as a critical indicator for Staphylococcus aureus infections, which can lead to serious health complications including osteomyelitis, an infection of the bone.
Published in the journal mBio, the study reveals that CCL20 levels increase significantly after infection, providing a promising avenue for early detection and treatment of these debilitating conditions. This breakthrough could be particularly beneficial for the approximately 2 million joint replacement surgeries performed annually in the United States, where infections remain a dreaded complication.
Understanding the Role of CCL20
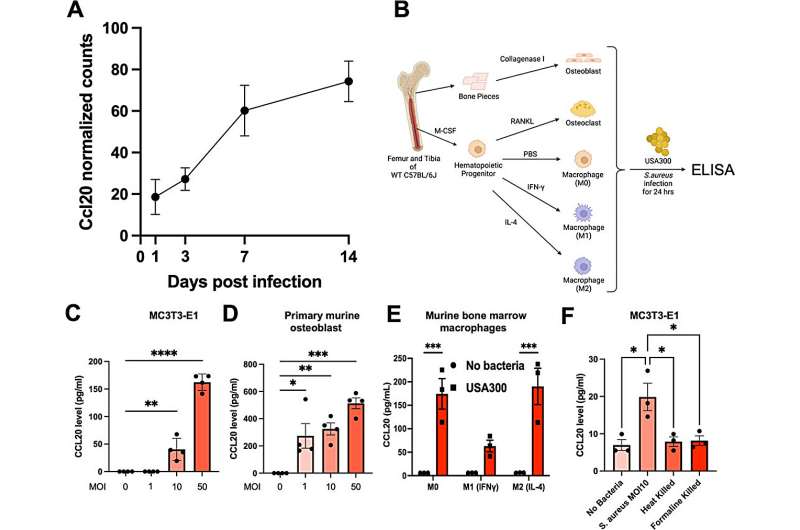
The research team explored how CCL20 functions in the body during staph-induced bone infections in mice. They discovered that CCL20 levels rose steadily after infection, and mice lacking this chemokine experienced more severe infections. This suggests that CCL20 plays a vital role in the immune response, helping the body to combat infections more effectively.
In a notable finding, healthy patients who had undergone hip or knee replacements showed normal levels of CCL20. However, those who developed bone infections exhibited a fivefold increase in the protein, while levels soared to 100 times normal in patients who succumbed to sepsis. This points to CCL20’s potential as an early warning system for the immune response to infections.
Gowrishankar Muthukrishnan, Ph.D., an assistant professor at the University of Rochester’s Center for Musculoskeletal Research, emphasized the urgency of treating staph infections promptly to enhance patient outcomes and reduce the risk of severe complications like sepsis. He stated, “There is no satisfactory treatment or diagnostic test for bone infection… it would be a huge advantage for surgeons if we could use a simple blood draw to measure CCL20.”
The Financial and Health Implications
The rising number of joint replacement surgeries has heightened concerns over post-operative infections, which can lead to significant health challenges. Although the percentage of patients who develop infections is relatively low, the consequences can be dire, resulting in prolonged antibiotic treatments and the need for additional surgeries.
Current estimates suggest that by 2030, there may be up to 200,000 prosthetic joint infections annually, leading to projected healthcare costs of $3 billion each year. This underscores the pressing need for effective diagnostic tools and treatments in managing bone infections.
According to Himanshu Meghwani, Ph.D., a staff scientist involved in the research, CCL20 could also be harnessed as a therapeutic agent. By attracting immune cells to the site of infection, CCL20 may bolster the body’s natural defenses. However, further research is needed, as some patients with elevated CCL20 levels still struggle to overcome infections.
The implications of this research extend beyond just improving patient care; they highlight a significant opportunity to shift how bone infections are diagnosed and treated, paving the way for better outcomes and potentially saving lives.
As the healthcare community continues to grapple with the challenges posed by bone infections, the findings surrounding CCL20 offer a glimmer of hope for advancements in diagnosis and treatment strategies.