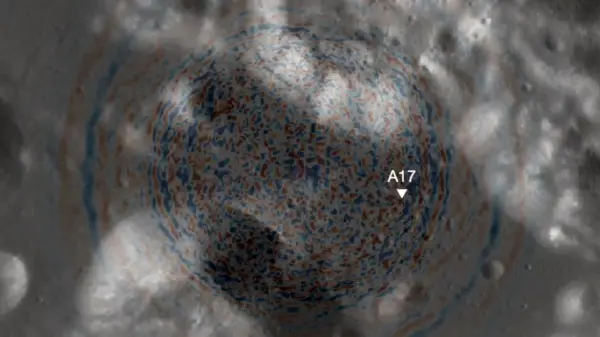
The diagnosis of diffuse midline gliomas is evolving with the integration of advanced biopsy techniques, biomarker testing, and coordinated pathology efforts. These tumors, often found in challenging areas such as the midbrain, pons, and brainstem, require careful handling to conserve limited biopsy tissue. Given the complexities surrounding their diagnosis, strategies are emerging that optimize both immediate clinical needs and long-term analytical value.
Balancing Immediate Needs with Long-Term Value
One of the key challenges in diagnosing diffuse midline gliomas is the preservation of biopsy tissue due to the inaccessibility of tumor locations. The reliance on immunohistochemical stains to identify histone mutations or loss of trimethylation can quickly deplete available material. As a result, medical professionals are turning to comprehensive next-generation sequencing (NGS) panels that can analyze hundreds of genes, including those commonly associated with these tumors. This method is increasingly recognized as a more reliable diagnostic approach.
Innovations in liquid biopsy techniques are also providing new avenues for diagnosis. The ability to sequence samples from cerebrospinal fluid (CSF) allows for the detection of pathognomonic histone mutations, presenting a less invasive option for some patients. Such advancements are crucial in community practices, where access to advanced molecular testing may be limited.
Strengthening Collaborations for Better Outcomes
Establishing partnerships with academic centers or external sequencing companies is essential for community practices facing challenges in managing biopsy samples. These collaborations should be proactive, allowing healthcare providers to be prepared for future cases rather than responding reactively. The initiation of molecular testing often falls to pathologists, although neuro-oncologists or neurosurgeons may sometimes assume this responsibility.
Preservation of tissue is critical for effective sequencing. Running through immunohistochemical stains, such as those for GFAP, P53, or KI67, can significantly reduce the available DNA for NGS, potentially compromising diagnostic accuracy. Therefore, clear communication between community and referral centers is vital to ensure that precious biopsy material is utilized effectively.
Technological advancements now enable sequencing with minimal DNA input, sometimes as low as 30–40 nanograms. While many academic institutions maintain in-house molecular testing capabilities, community practices can still contribute unstained slides suitable for sequencing if full tissue blocks cannot be sent. These innovations can help overcome logistical barriers and minimize the risk of obtaining non-diagnostic results.
By effectively conserving biopsy tissue, coordinating with pathology labs, and utilizing modern sequencing platforms, both academic and community healthcare settings can achieve more timely and accurate diagnoses for patients facing the challenges of diffuse midline gliomas. This coordinated approach is essential in improving patient outcomes and advancing the field of neuro-oncology.