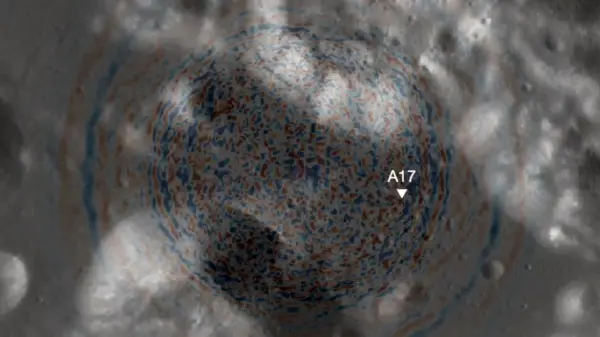
Research into chimeric antigen receptor-modified T cell (CAR-T) therapy targeting GD2 is advancing as a potential treatment for patients with diffuse midline gliomas characterized by H3K27M mutations. Early-phase clinical trials indicate that directing engineered T cells to attack tumor-specific markers can yield significant radiographic responses. Nevertheless, several challenges persist, particularly regarding the optimal delivery methods for these therapies.
As researchers explore methods of administering CAR-T cells, they are considering various approaches, including systemic delivery, direct injection into the tumor cavity, and infusion into the cerebrospinal fluid. Initial studies have reported rapid responses to treatment, but these effects are often transient. Moreover, the regimens have been associated with considerable toxicities, notably severe inflammation that may necessitate intensive care and cerebrospinal fluid diversion procedures.
Safety concerns dominate the application of CAR-T therapy in treating diffuse midline gliomas, especially in pediatric patients with brainstem tumors like DIPG. In these cases, even minimal inflammation or edema resulting from treatment can pose life-threatening risks due to the tumor’s critical location. To address these issues, researchers have developed a specialized toxicity grading system known as tumor inflammation-associated neurotoxicity. This system aims to enhance the characterization and management of treatment-related risks.
In contrast, adult glioblastoma cases, characterized by tumors in less confined regions of the brain, exhibit different toxicity profiles. While the risks remain significant, the location of these tumors allows for more flexibility in treatment approaches. The challenge lies in balancing the potential therapeutic benefits of CAR-T therapy against the risk of severe complications.
Despite the risks, results from CAR-T trials have documented not only short-lived responses but also occasional durable partial and complete remissions. These findings underscore the potential of CAR-T therapy as a viable treatment option, even amid the complexities involved. As the therapeutic landscape evolves, there is a pressing need to identify biomarkers that can accurately predict which patients are most likely to benefit from this treatment.
Advancements in biomarker identification could transition CAR-T therapy from an experimental intervention to a more targeted component of treatment for diffuse midline gliomas. The promise shown in early studies highlights the importance of continued research and innovation in this field, as the quest to improve outcomes for patients with challenging diagnoses continues.