Chronic venous insufficiency (CVI) affects up to 40% of adults in the United States, a condition where the leg veins struggle to return blood to the heart. Dr. Miguel F. Manzur, a vascular surgeon at the USC Cardiac and Vascular Institute, part of Keck Medicine of USC, provides essential insights into CVI, its symptoms, risk factors, and treatment options.
What is Chronic Venous Insufficiency?
CVI occurs when the valves in the leg veins fail to function properly. This malfunction hinders blood from moving upwards, causing it to pool in the lower legs. The most common symptoms include swelling, a feeling of heaviness or fatigue in the legs, and visible varicose veins. Over time, individuals may also experience skin discoloration and even ulceration. The primary symptom reported by patients is typically leg swelling.
Risk Factors for Development
Several factors can increase the likelihood of developing chronic venous insufficiency. Aging is a significant risk; individuals over the age of 50 are more susceptible. Women are particularly affected due to hormonal changes during pregnancy, which increase blood volume and can strain the veins.
Genetics also play a crucial role; those with family histories of vein issues, such as a mother or aunt with similar problems, are at higher risk. Additional factors include obesity and a sedentary lifestyle, both of which can disrupt normal blood flow. A history of deep vein thrombosis (DVT), where a blood clot forms in a deep vein, further elevates the risk of developing CVI.
Diagnosis of Chronic Venous Insufficiency
Diagnosing CVI begins with a thorough physical examination. Doctors assess the legs for signs such as spider veins or significant swelling. To confirm the diagnosis, a venous reflux ultrasound is performed, a noninvasive test that evaluates the functionality of the valves in the veins. If blood is found to flow backward, this indicates faulty valves, confirming chronic venous insufficiency.
Treatment Options Available
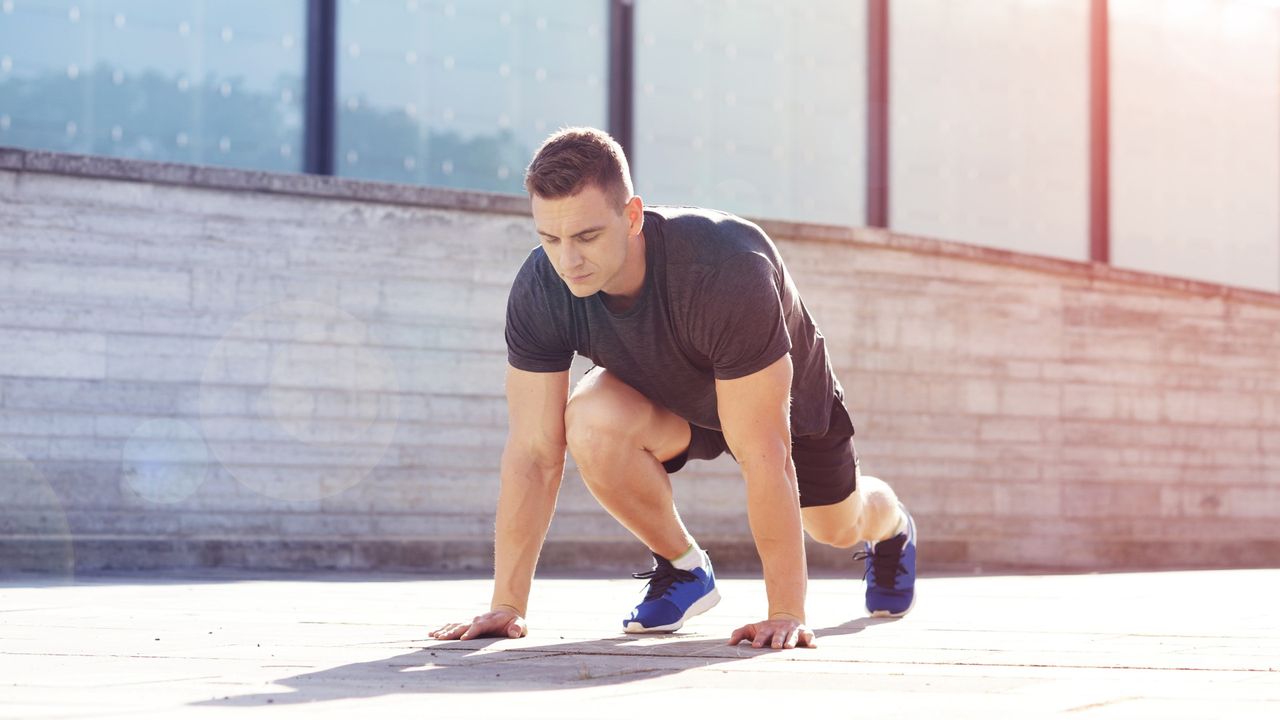
Treatment for CVI varies based on its severity. For many, the condition presents as an inconvenience, characterized by heavy or tired legs. In such cases, lifestyle changes are recommended. Dr. Manzur suggests regular walking to help the leg muscles pump blood effectively. Additionally, losing weight and elevating the legs can alleviate swelling.
Compression stockings are a common first-line treatment, providing support to the veins and improving blood flow. For patients with more severe symptoms, such as those experiencing skin discoloration or ulcerations, proper wound care is essential to prevent infections. In some instances, doctors may prescribe diuretics or topical steroids for skin irritations.
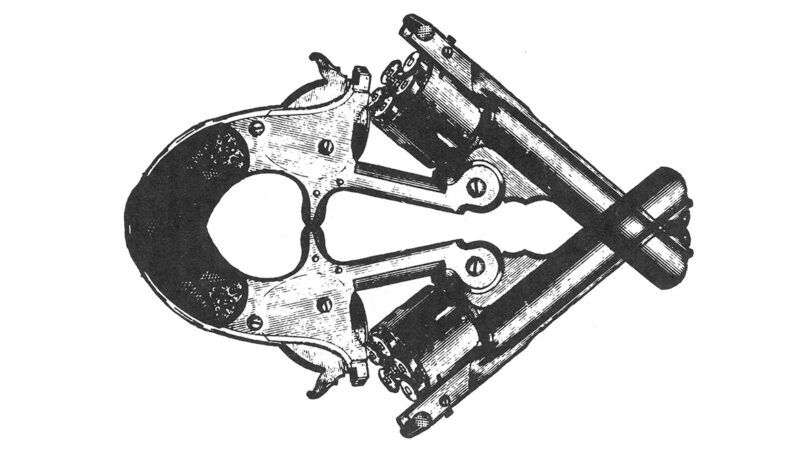
If conservative measures fail to relieve symptoms, more advanced treatments may be necessary. Options include venous ablation, a minimally invasive procedure to remove the damaged vein, which typically lasts 20–30 minutes and allows patients to go home the same day. Other procedures, such as stenting or phlebectomy, may also be performed in an office setting.
Long-Term Management and Travel Considerations
CVI is a chronic condition that can recur. While treatments can be effective and long-lasting, new varicose veins may develop, particularly after ulcerations. Maintaining regular communication with a vein specialist is advisable for ongoing management, especially for those with more extensive disease.
Traveling can worsen symptoms due to prolonged sitting, which exacerbates leg swelling and discomfort. Dr. Manzur recommends wearing compression socks and taking breaks every hour to walk around, promoting blood circulation. While seated, performing calf exercises can also aid in blood flow.
In summary, chronic venous insufficiency is a prevalent condition that significantly affects many adults. Understanding its symptoms, risk factors, and management strategies can empower individuals to take proactive steps toward their vascular health.