President Donald Trump and congressional Republicans have initiated a significant push for reform in the U.S. health insurance system as many Americans embrace resolutions to improve their health in 2026. Congressional committees are preparing to scrutinize insurance executives, focusing on practices that contribute to rising healthcare costs. The administration aims to apply direct pressure on these executives to reduce insurance premiums, recognizing that the systemic issues within health insurance are central to broader healthcare challenges.
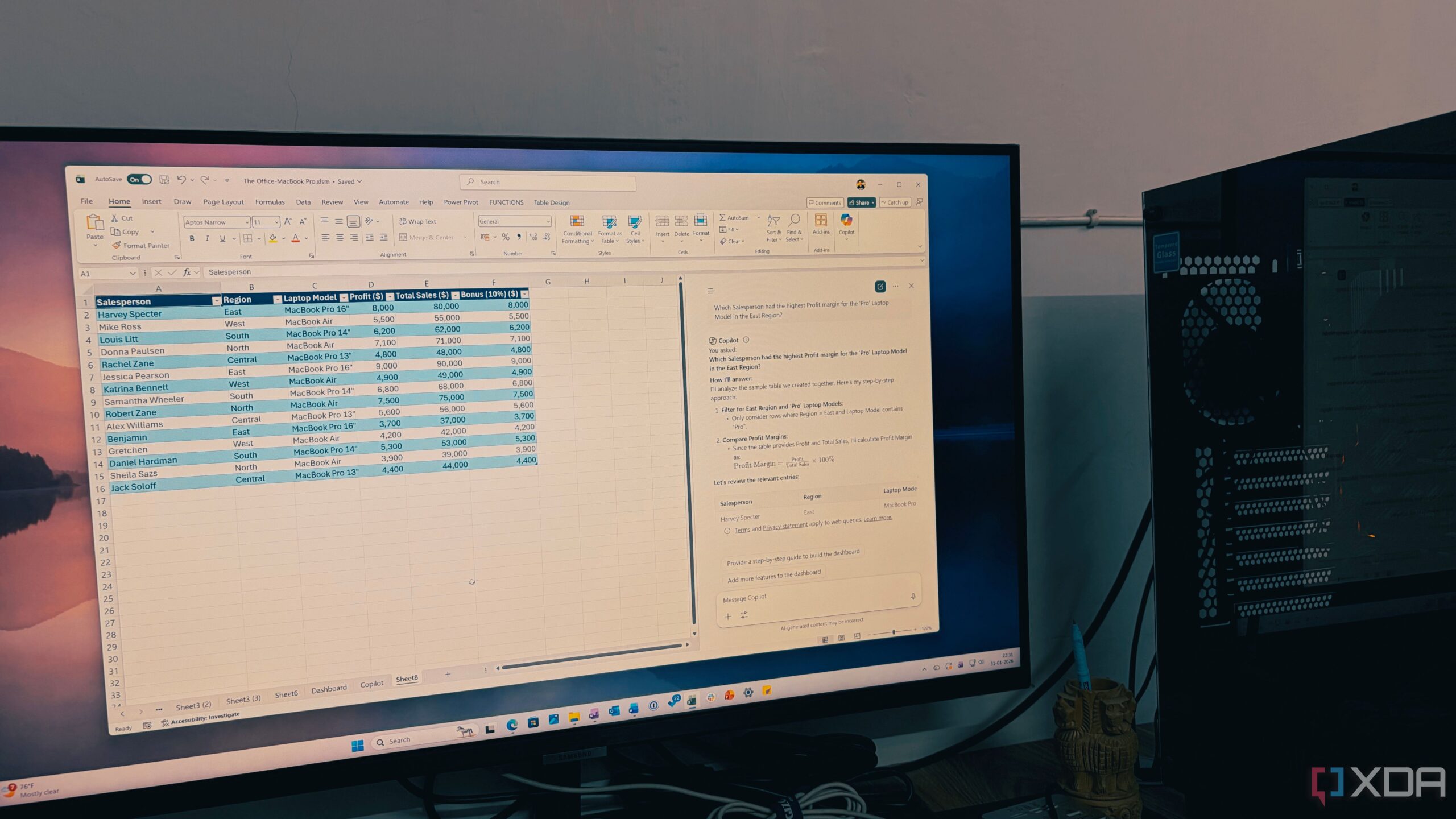
The current health insurance landscape has become increasingly complex, with insurers having substantial control over medical decisions. They determine which services patients can access, where treatment occurs, and the medications prescribed, effectively influencing the cost of care. Despite widespread acknowledgment of the detrimental impact of insurers, the system has evaded meaningful reform for years. Instead, it has been sustained by significant taxpayer subsidies, often supported by politicians with close ties to the industry.
As the cost of healthcare continues to rise, the average family plan for two adults and two children on the Obamacare exchanges now costs nearly $27,000 annually in premiums. With healthcare costs outpacing wage growth, projections suggest that by 2032, the average American family could spend an alarming 40% of its income on health premiums.
The issues extend beyond financial burdens. As a former clinician, Dr. Wolfgang Klietmann points out, the expanding reach of insurers increasingly undermines the clinical judgment of healthcare providers. Insurers often override doctors’ recommendations, dictating the medications and treatments patients can access. Furthermore, pharmacy benefit managers (PBMs) frequently direct patients towards higher-cost medications that generate greater rebates for insurers, leading to increased out-of-pocket expenses for patients, even when more affordable alternatives exist.
Insurers are also exploiting loopholes through the creation of offshore entities known as Group Purchasing Organizations (GPOs). This practice enables them to evade U.S. tax liabilities and sidestep requirements that would ordinarily mandate passing negotiated rebates on to patients, resulting in higher costs at the pharmacy counter.
To achieve genuine reform, Congress must implement structural changes to the health insurance system. Key steps include curbing the power of insurers and PBMs by eliminating incentives to inflate drug prices and enhancing transparency regarding coverage decisions. It is also crucial to stop the flow of taxpayer dollars into a system marked by fraud and waste; last year, the federal government allocated nearly $140 billion to subsidize Obamacare, yet taxpayer subsidies per enrollee have increased by over 50% since 2014 without corresponding improvements in care or affordability.
The misuse of taxpayer funds is evident in the offerings of Medicare Advantage plans that include non-medical perks, such as ski passes and pet food, at the expense of essential health services. The Paragon Institute has estimated that over 6 million individuals received fully subsidized Obamacare coverage last year despite ineligibility. Moreover, the Centers for Medicare & Medicaid Services revealed that nearly 3 million Americans were improperly enrolled in multiple plans in 2024, leading to duplicated payments for care.
The healthcare system’s complexities and abuses often mirror the historical criticisms raised by Émile Zola regarding government complicity in fraud and concealment. Today, a similar dynamic appears to exist, as government officials, policymakers, and insurers remain intertwined in reimbursement practices that elevate costs for patient care.
While both the United States and Europe rely on the same pharmaceutical manufacturers for life-saving medications, American patients frequently face higher prices for identical drugs. This discrepancy is not due to differences in the medications themselves but arises from the layers of fees, rebates, and opaque pricing structures imposed by insurers and intermediaries.
To reduce dependency on taxpayer-funded insurance for all aspects of healthcare, it is essential to empower patients with greater control over their medical choices. Expanding the use of health savings accounts could allow individuals to manage their healthcare expenditures directly, without needing to navigate insurer approvals.
As President Trump and his congressional allies embark on this ambitious reform journey, patients are hopeful for a health insurance landscape that prioritizes their needs and well-being. The call for reform is urgent, and the outcome will significantly impact how Americans access and afford healthcare in the years to come.