A team of scientists has developed a new snake bite antivenom that effectively targets a wide range of venomous snake species. This innovative antivenom can potentially save thousands of lives each year by providing a treatment option for 17 different species of snakes, particularly those in the deadly Elapidae family.
Advancements in Antivenom Technology
The study, published in the journal Nature, highlights the ability of the new antivenom to counteract venom from several dangerous snakes, including cobras and mambas. According to Anne Ljungars, a biological engineer at the Technical University of Denmark and co-author of the study, the antivenom specifically targets 17 of the 18 elapid species found in Sub-Saharan Africa. Each year, the region records over 300,000 snake bites, resulting in approximately 7,000 fatalities.
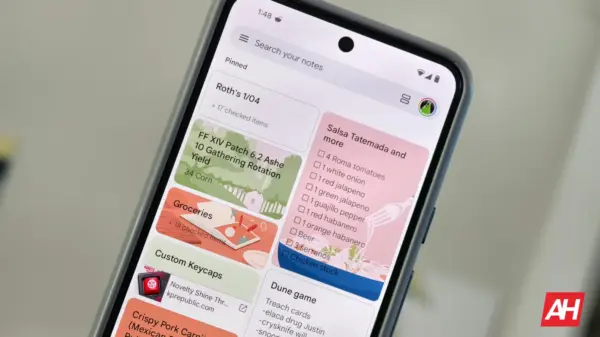
Current antivenoms often require victims to identify the snake species that caused the bite, a task that can be challenging during a medical emergency. Traditional production methods for antivenoms have remained largely unchanged since the 1800s, relying on the immunization of horses with snake venom to extract antibodies. This process yields a variable mixture of antibodies, resulting in products that can have serious side effects.
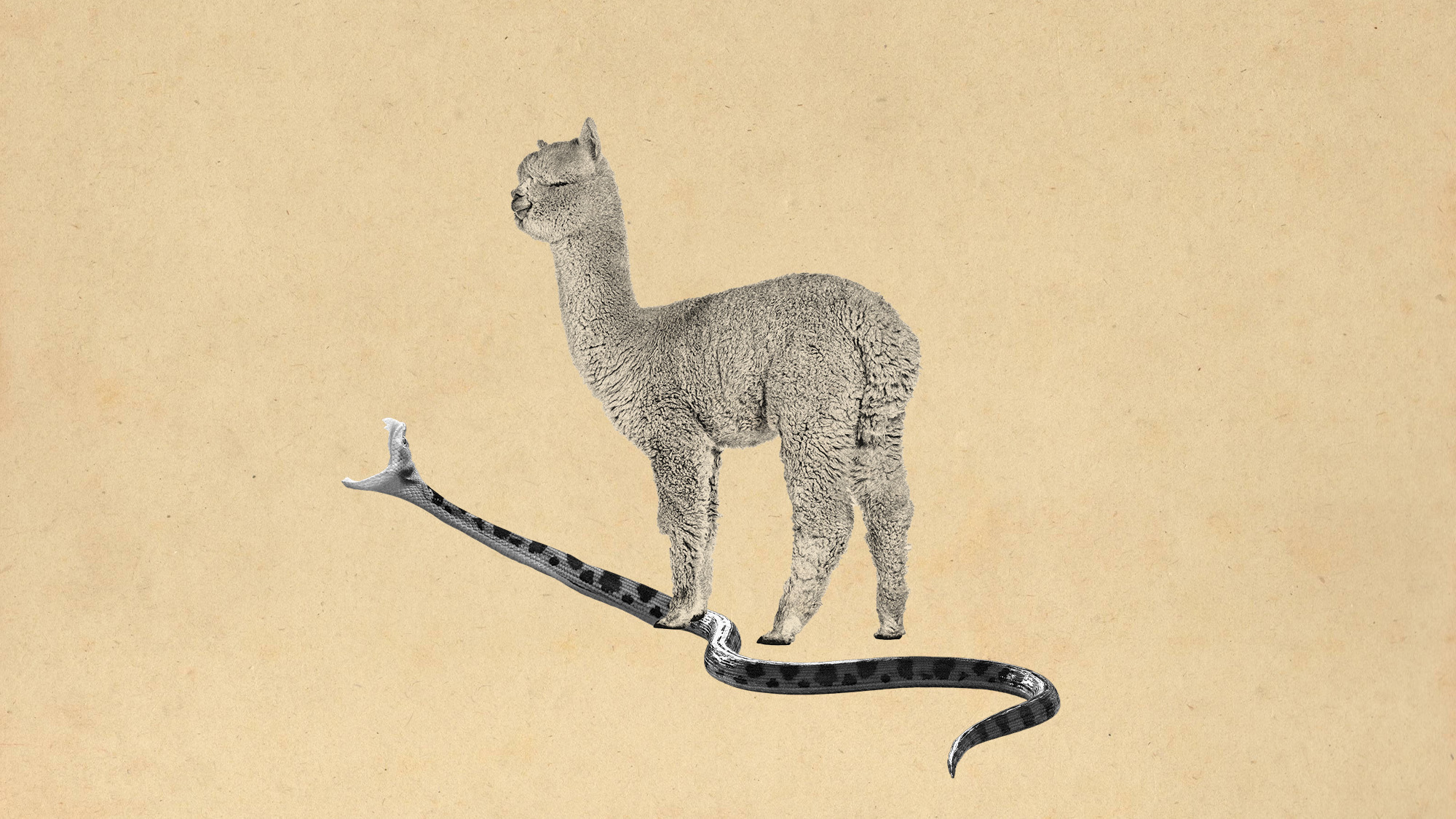
Innovative Use of Camelid Antibodies
The researchers turned to camelids, such as alpacas and llamas, which possess unique immune systems capable of producing a special type of antibody known as heavy-chain-only antibodies. These antibodies can be engineered into nanobodies, which are smaller and more stable than standard antibodies. As explained in the study’s news release, nanobodies can bind strongly and precisely to various toxins, enabling the antivenom to neutralize venom from multiple snake species.
The new antivenom demonstrates a promising safety profile, with reports indicating it “almost always prevented tissue death at the injection site.” This is a significant improvement over existing products, which can lead to severe complications, including limb amputations. The nanobodies also penetrate tissues more effectively and can be administered in remote locations, as they can withstand freeze-drying and do not require refrigeration.
While initial tests in mice show encouraging results, the antivenom has yet to be evaluated in human subjects. Additionally, researchers note that its effectiveness decreases when administered after venom exposure, and the venom from certain species was only partially neutralized.
Despite these limitations, the study offers promising evidence for the potential of nanobody mixtures as a new therapeutic approach to snakebite treatment. Nicholas Casewell, director of the Centre for Snakebite Research and Interventions at the Liverpool School of Tropical Medicine and co-author of the study, emphasized the importance of this research in providing a potentially life-saving solution for snake bite victims.