A recent case in Long Island, New York, has raised alarms regarding the spread of mosquito-borne diseases in the United States. A woman fell ill with chikungunya, a virus typically associated with regions in East Africa, Latin America, and Southeast Asia. Notably, she had not traveled abroad, highlighting the concerning trend of diseases once confined to tropical regions now appearing in the U.S.
The emergence of chikungunya in New York is part of a broader pattern. Diseases that were historically limited to warmer climates are increasingly becoming a public health concern in the U.S. Over the past few years, the incidence of dengue virus, commonly known as breakbone fever, has surged significantly. In 2022, more than 6,500 locally acquired cases were reported, predominantly in Puerto Rico, but also in the U.S. Virgin Islands, Florida, California, and Texas. This figure marks a sharp increase from historical data, indicating a rising threat.
These mosquito-borne illnesses can have severe consequences. They place immense strain on healthcare systems, disrupt daily life, and can be life-threatening, especially for vulnerable populations such as young children and the elderly. The economic impact is staggering; in Latin America and the Caribbean, dengue is estimated to cost between $1.7 billion and $3 billion annually.
Lessons from Latin America and the Caribbean
According to the Pan American Health Organization (PAHO), countries in Latin America and the Caribbean have long grappled with these public health challenges and have developed effective strategies to manage them. The experience gained from these regions provides valuable lessons for the U.S. in tackling similar threats.
Warming temperatures, urban expansion, and the adaptation of mosquito species are creating ideal conditions for outbreaks. If not addressed swiftly, the spread of these diseases could lead to serious repercussions for public health and the economy in the United States.
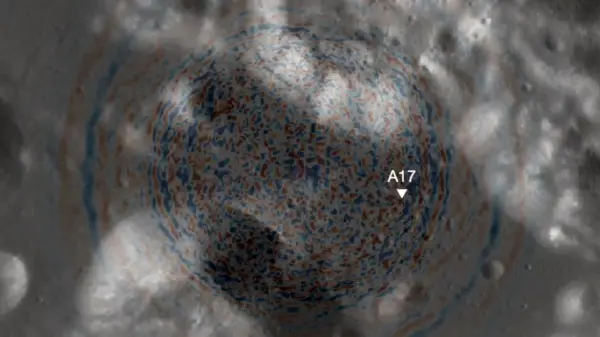
To prepare for potential outbreaks, PAHO emphasizes several key strategies. First, enhancing disease surveillance is critical. Robust tracking systems are essential for monitoring the geographic spread of diseases and the insects that transmit them. Such systems can generate actionable data, allowing for rapid responses and collaborative efforts across cities, states, and even countries.
For instance, a recent chikungunya outbreak in Paraguay demonstrated the importance of timely alerts. The outbreak was marked by severe symptoms and unexpected fatalities among children, underscoring the need for vigilance and preparedness.
Training and Collaboration are Essential
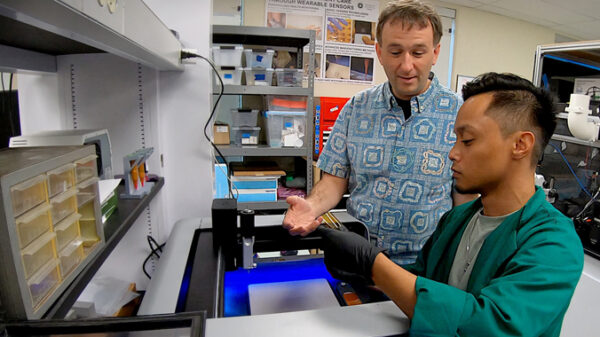
Another vital component is training healthcare workers to recognize early warning signs of these diseases. Quick clinical responses can save lives, as many cases go undetected until they escalate. From primary care clinics to hospitals, healthcare providers must be equipped to identify symptoms, confirm diagnoses through laboratory testing, and ensure patients receive timely care.
Since 2011, PAHO has trained over 740,000 healthcare workers across the Americas to manage insect-borne diseases, including dengue and chikungunya. This initiative has been instrumental in preventing over 7,000 dengue-related deaths in the region. As new areas face increased risk, ongoing training will be crucial.
Furthermore, international cooperation is paramount. Mosquitoes do not recognize borders, and their movement facilitates the spread of diseases. Collaborative efforts, such as data sharing and coordinated surveillance responses, are essential in combating the threat of these diseases effectively.
Despite a record number of dengue cases in the region last year, fewer than 1 percent of those infected died—a testament to the effectiveness of regional preparation and rapid response.
The recent appearance of chikungunya in New York should prompt concern but not panic. By adopting successful strategies from Latin America and the Caribbean, the U.S. can bolster its defenses against mosquito-borne diseases. It is imperative to leverage the latest data, foster international cooperation, and learn from the expertise of communities that have successfully faced these challenges for generations.
Jarbas Barbosa, director of the Pan American Health Organization and regional director for the Americas at the World Health Organization, emphasizes that taking these proactive measures will significantly contribute to safeguarding the health and security of the American populace.