A recent comprehensive review of medical cannabis use over the past 15 years has raised significant doubts about its effectiveness for treating various conditions. The analysis indicates that while millions of Americans use cannabis for pain relief, anxiety, and sleep issues, the evidence supporting its benefits is often weak or inconclusive. This review, led by Dr. Michael Hsu, an addiction psychiatrist at the University of California, Los Angeles, was published in the medical journal JAMA last month.
The study examined over 2,500 clinical trials, guidelines, and surveys primarily conducted in the United States and Canada. Researchers found a disparity between the health issues for which patients seek cannabis and what rigorous scientific research indicates regarding its effectiveness. Nearly 30 percent of individuals using medical cannabis were found to meet the criteria for cannabis use disorder, highlighting potential risks associated with its consumption.
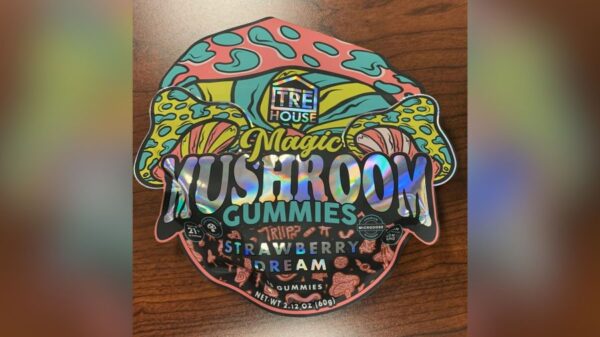
Despite the growing acceptance of cannabis products, which now represent a thriving $32 billion industry, the review suggests that the medical community lacks a solid understanding of medical cannabis. A 2021 review cited in the study revealed that only 33 percent of clinicians internationally felt confident in their knowledge of medical cannabis, with a staggering 86 percent expressing the need for further education.
Insights from Research and Guidelines
The review made a clear distinction between medical cannabis, which is sold at dispensaries, and pharmaceutical-grade cannabinoids. The latter includes FDA-approved medications like Marinol, Syndros, and Cesamet, which have demonstrated effectiveness in alleviating chemotherapy-related nausea, stimulating appetite in patients with severe conditions like H.I.V./AIDS, and addressing certain pediatric seizure disorders.
Despite the prevalent use of cannabis for pain management, the review found no substantial evidence indicating that it alleviates acute pain. It referenced the guidelines from the American Society of Clinical Oncology issued in 2024, which state that there is insufficient evidence for or against recommending cannabis specifically for cancer-related pain.
The findings from this review come at a time when the normalization of cannabis products continues to rise. As more patients turn to cannabis for relief, the medical community faces the challenge of ensuring that healthcare providers are adequately informed about the potential benefits and risks associated with its use. The review underscores the need for further research and education to bridge the gap between public perception and scientific evidence regarding medical cannabis.