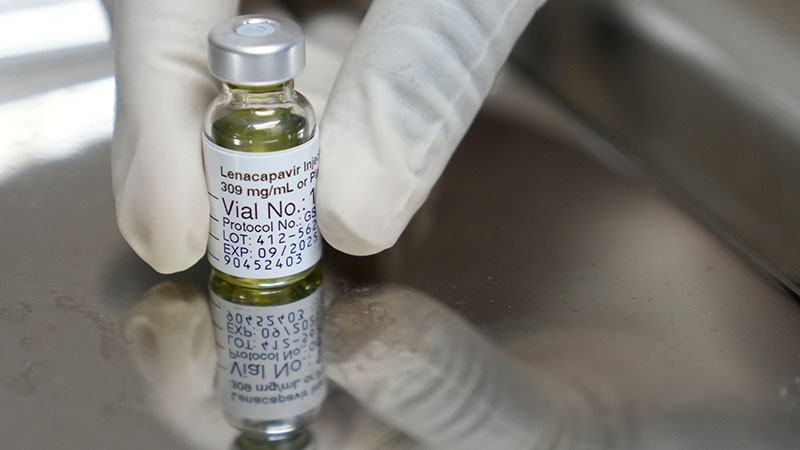
Advocates for HIV prevention have hailed the recent approval of a new injectable medication, lenacapavir, marketed under the brand name Yeztugo, as a significant advancement in efforts to curb the virus’s spread. Approved by the U.S. Food and Drug Administration (FDA) this summer, lenacapavir demonstrated remarkable efficacy in clinical trials, nearly eliminating HIV transmission among participants. Unlike traditional daily oral PrEP (pre-exposure prophylaxis), this innovative treatment is administered via injection just twice a year.
Christopher Hamilton, CEO of Texas Health Action, which operates the Kind Clinic in Austin, expressed optimism about the new treatment. He stated, “This new injectable PrEP for HIV prevention is going to be a game changer for a lot of people.” According to Hamilton, the twice-yearly injection schedule could significantly improve adherence for individuals who struggle with daily medications.
Overcoming Barriers to Access
Hamilton highlighted that for many, especially those facing housing instability, taking a daily pill can be a substantial challenge. “You don’t have to remember a pill every single day,” he noted, emphasizing the potential for lenacapavir to remove barriers that have historically hindered effective HIV prevention.
The Kind Clinic is currently developing protocols to administer the injection, although Hamilton mentioned that a timeline for implementation has yet to be established. A pressing concern remains the cost of the drug, which has a list price exceeding $14,000 per injection. Insurance coverage for lenacapavir is still evolving, and Hamilton explained that patients may need a medical exception from their doctor to secure coverage.
“Right now, it does take a medical exception, meaning your doctor has to write to the insurance company and detail the reasons why this injectable version is better for the patient than daily oral medication,” he added. While many insurance plans currently cover daily oral PrEP, it may take time for them to adapt to the new injectable option.
Community Support and Future Prospects
The Kind Clinic benefits from community support, including funding from the Hill Country Ride for AIDS, an annual event that raises funds for various Central Texas organizations providing HIV/AIDS services. Scheduled for April 18, 2026, the ride exemplifies local commitment to combating the epidemic. Eli Oldham, ride director, noted the event’s long-standing impact, stating, “I’ve been lucky to be part of it for so many years.”
Oldham expressed hope that the costs associated with lenacapavir will decrease over time, similar to the trend observed when oral PrEP medications were first introduced. “When PrEP and all those medications first started hitting the market, they were also really expensive,” he remarked. “Hopefully, we’re in a shorter game now.”
Hamilton echoed this sentiment, acknowledging that while the current price is prohibitive for many organizations, there is optimism for future accessibility. “It’s going to take us some time to figure out at what price we could purchase this medication,” he said, adding that the manufacturer plans to offer a patient assistance program for uninsured individuals.
The administration of lenacapavir must be conducted by a healthcare provider in a medical facility or specialty pharmacy. Hamilton pointed out that the Kind Clinic is uniquely positioned, as it has pharmacies within two of its Austin locations, allowing for on-site administration of the medication. “But you won’t be able to just go to your local pharmacy, take it home, and do the injection yourself,” he clarified.
Clinical Trial Success and the Importance of Care
Clinical trials for lenacapavir have shown it to be highly effective in preventing HIV. Participants, including gay and bisexual men and transgender individuals at risk for HIV, either received lenacapavir injections every six months or took daily Truvada, a well-known oral PrEP medication. The results indicated that lenacapavir was 89% more effective at preventing HIV transmission than the daily option.
For both Hamilton and Oldham, the introduction of this new prevention method symbolizes not only medical progress but also renewed hope for those affected by HIV. Hamilton urges individuals not currently connected to care to take proactive steps: “If you haven’t established care with a clinic, start now. Know your status, have a routine for your sexual health.”
Oldham encapsulated this sentiment, stating, “Anytime there’s a breakthrough or new treatment for HIV, it’s exciting because it’s always about the progress that’s coming.” As the healthcare community prepares for the rollout of lenacapavir, the focus remains on expanding access and support for individuals at risk of HIV, marking a pivotal moment in the ongoing fight against the virus.