Concerns over immigration raids are prompting a significant decline in patient visits to healthcare facilities, pushing many to seek telehealth services instead. Pediatrician Jacob Sweidan, who has served low-income families in Southern California for four decades, reported unprecedented levels of patient fear, stating, “They are scared to come to the offices. They’re getting sicker and sicker.” The impact of heightened immigration enforcement is evident as families, including those with U.S. citizen children, retreat from seeking necessary medical care.
In recent months, the atmosphere surrounding healthcare access has deteriorated following actions by the Trump administration to rescind protective measures for sensitive areas. These changes have led to a notable increase in patients avoiding clinics due to fears of deportation. Health experts, including Sara Rosenbaum, a professor emerita at George Washington University, have indicated that clinics across the nation are witnessing a drop in in-person visits among immigrant populations.
Shifting Strategies in Healthcare Delivery
To adapt to these challenges, many healthcare providers are reintroducing telehealth services, which had declined following the COVID-19 pandemic. Jim Mangia, president and CEO of St. John’s Community Health, shared that virtual visits have surged from 8% to approximately 25% of all appointments. This shift comes as clinics employ creative strategies to ensure that vulnerable populations, including undocumented immigrants, receive care. St. John’s serves around 30,000 individuals without legal status annually, highlighting the critical need for flexible healthcare solutions.
Patients are increasingly reluctant to pick up prescriptions or attend routine appointments due to fears stemming from recent federal actions. Reports indicate that federal agents have attempted to access patients in mobile clinics, raising concerns among clinic staff about the safety of their patients.
One patient, identified only as C.S. for her safety, expressed her anxiety about seeking care, stating, “I feel so worried because if I don’t get the care I need, it can get much worse.” This sentiment is echoed by many in the community, underscoring a broader “fear pandemic” affecting immigrant families.
Community Responses and Legislative Measures
Los Angeles County officials have responded to the growing crisis by exploring options to expand virtual appointment availability. The county’s director of health services has reported a substantial increase in phone and video consultations, reflecting the urgent need for accessible care. Additionally, state lawmakers are considering legislation to restrict immigration agents from accessing schools and healthcare facilities, further emphasizing the need for protective measures.
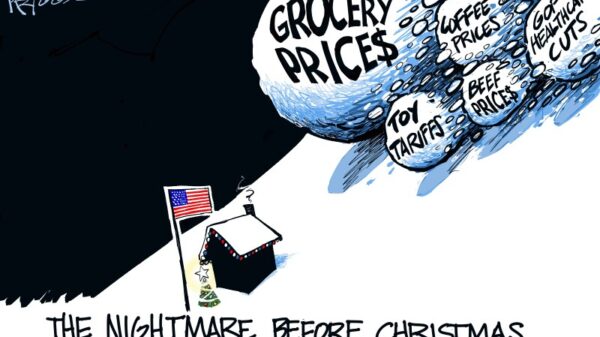
Healthcare providers are bracing for increased demand as patients avoid preventive care, leading to more severe health issues that require expensive emergency interventions. Nicole Lamoureux, president of the National Association of Free & Charitable Clinics, warned that cuts to Medicaid will only exacerbate the strain on emergency services.
Community health centers, such as the Venice Family Clinic, have begun proactive outreach efforts, calling patients to confirm their attendance and offering telehealth as an alternative for those hesitant to visit in person. The clinic has reported a 5% rise in telehealth visits over the past month, illustrating the shift in how healthcare is being delivered amidst ongoing fears.
In the Salinas Valley, efforts to promote telehealth through Spanish-language radio ads have begun, while CalOptima Health has sent over a quarter-million text messages encouraging patients to utilize telehealth services. These initiatives aim to mitigate the barriers that many patients face, particularly in immigrant communities.
As the situation progresses, healthcare providers remain concerned about the long-term implications of relying solely on telehealth. Isabel Becerra, CEO of the Coalition of Orange County Community Health Centers, emphasized that while telehealth can serve as a temporary solution, it cannot substitute for in-person care, especially for procedures requiring lab work or physical examinations.
The fear surrounding immigration raids is not limited to those without legal status. Residents, including naturalized citizens, also express anxiety about seeking care. One patient, identified as V.M., described feeling paranoid when venturing outside, highlighting the pervasive climate of fear affecting various demographics.
Overall, the current healthcare landscape reflects a complex interplay of immigration policy, community health needs, and the adaptation of healthcare delivery methods. As families navigate this challenging environment, the long-term effects on public health and access to care remain to be seen. This evolving situation underscores the urgent need for comprehensive strategies to ensure that all individuals, regardless of their immigration status, can access the care they need.
This article was produced by KFF Health News, an independent source dedicated to providing in-depth journalism about health issues.