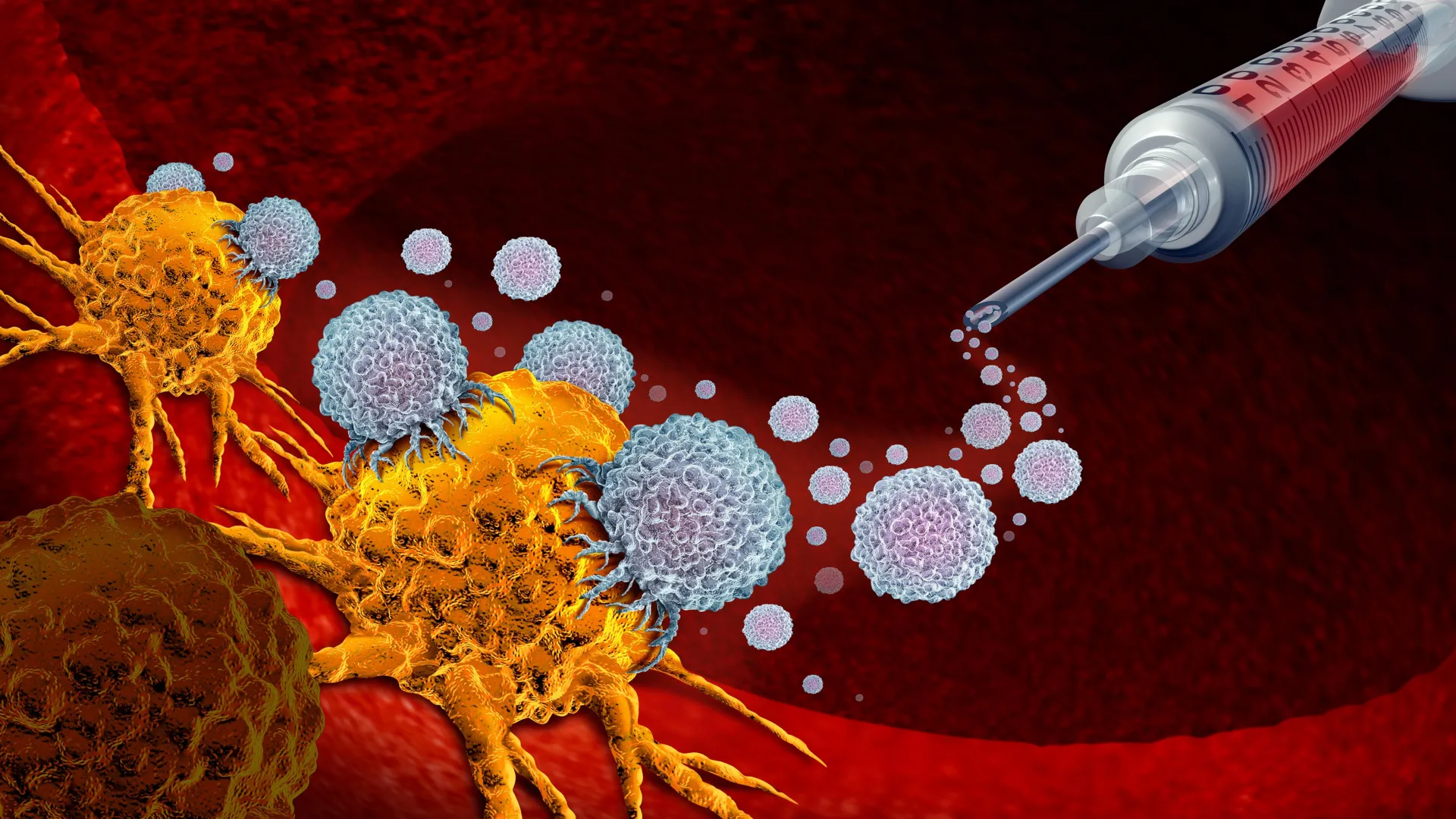
A groundbreaking study from Duke Health reveals that a cancer vaccine trial conducted over two decades ago may hold significant implications for long-term survival in breast cancer patients. Remarkably, every participant from the trial, which focused on advanced breast cancer, is still alive. This outcome is particularly striking given the typical prognosis for metastatic breast cancer, which often results in reduced survival rates.
The research, led by Dr. Herbert Kim Lyerly, a professor of immunology, examined the immune responses of women who received the experimental vaccine in the early 2000s. The findings demonstrated that these patients retained robust immune memory cells capable of recognizing and targeting their cancer. Specifically, the cells featured a marker known as CD27, which plays a crucial role in the immune system’s ability to remember past threats.
Innovative Approaches to Cancer Immunology
Published in the journal *Science Immunology*, the research highlights the potential of CD27 to enhance the effectiveness of cancer vaccines. Dr. Zachary Hartman, the study’s senior author, expressed surprise at the durability of the immune responses observed. “We were stunned to see such durable immune responses so many years later,” he noted. This discovery raises the question of whether it is possible to further amplify these immune responses.
To explore this, the research team conducted laboratory experiments using mice. They combined a vaccine targeting the HER2 protein, often associated with breast cancer, with an antibody that activates CD27. The results were promising; nearly 40% of the mice that received this combined treatment experienced complete tumor regression, compared to just 6% of those treated with the vaccine alone.
Reevaluating the Role of Immune Cells
This study shifts the focus from the traditionally emphasized CD8+ “killer” T cells to the often-overlooked CD4+ “helper” T cells. While killer T cells are recognized for their tumor-fighting capabilities, the research suggests that helper T cells may be equally important in developing lasting immune memory and bolstering the effectiveness of other immune cells.
When researchers introduced an additional antibody to support CD8+ T cells, the tumor rejection rate in mice soared to nearly 90%. “This study really shifts our thinking,” Hartman stated, emphasizing the critical role of CD4+ T cells in the immune response against cancer.
The findings also indicate that the CD27 antibody could be administered as a single dose alongside the vaccine, providing a straightforward enhancement to current treatment protocols. This simplicity could facilitate the integration of this approach with existing therapies, including immune checkpoint inhibitors and antibody-drug conjugates that are already in use.
Dr. Hartman believes that these advancements may finally unlock the full potential of cancer vaccines. “We’ve known for a long time that vaccines can work against cancer, but they haven’t lived up to the hype,” he explained. “This could be a missing piece of the puzzle.”
The study received funding from the National Institutes of Health and the Department of Defense, underscoring the significance of this research in the ongoing battle against cancer. As scientists continue to investigate these promising avenues, the hope for more effective cancer treatments becomes increasingly tangible.