A recent study highlights a critical global shortage of nearly 1 million midwives, which is jeopardizing the essential care needed to protect maternal and infant health. This gap is particularly severe in Africa, where 90% of women live in countries lacking adequate midwifery services. The research underscores the urgent need for enhanced midwifery support to prevent unnecessary maternal and neonatal deaths.
The findings were presented by the International Confederation of Midwives (ICM), with input from its chief executive, Anna af Ugglas. She stated, “Nearly 1 million missing midwives means health systems are stretched beyond capacity, midwives are overworked and underpaid, and care becomes rushed and fragmented.” The consequences of this shortage are dire, leading to increased intervention rates and a higher likelihood of poor-quality care for women and their babies.
To provide adequate care throughout pregnancy, childbirth, and the postpartum period, the study estimates that an additional 980,000 midwives are needed across 181 countries. Previous research indicates that universal access to midwife-led care could avert two-thirds of maternal and newborn deaths as well as stillbirths, potentially saving 4.3 million lives annually by 2035.
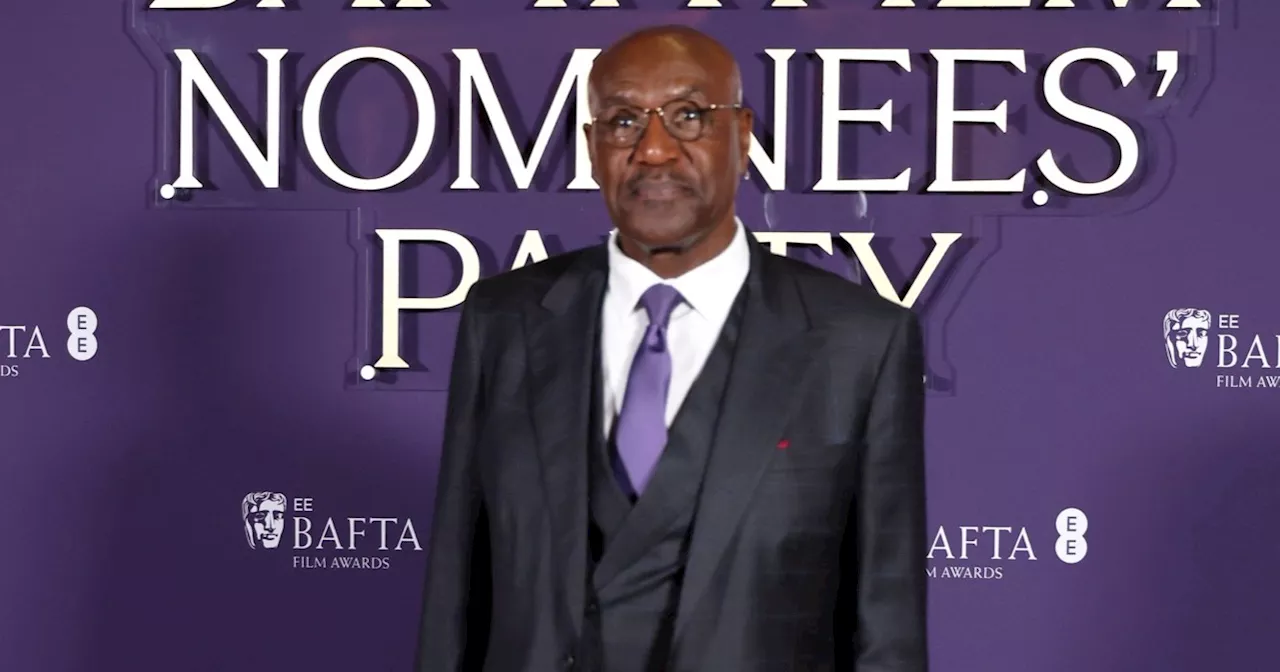
The ICM report emphasizes that the shortage is not merely due to a lack of training opportunities. It also reflects systemic failures in employing qualified midwives and retaining those already in the workforce. Professor Jacqueline Dunkley-Bent, the ICM’s chief midwife and co-author of the report, noted, “In many settings, midwives are educated but not absorbed into the workforce or not enabled to practice fully, compounding this already serious and universal shortage of midwives.”
The data reveals that more than 90% of the global midwife shortage exists in low- and middle-income countries. For instance, Africa has only 40% of the midwives it requires, while the eastern Mediterranean region has a mere 31%. The Americas are in a better position but still only have 15% of the needed workforce. Shortfalls, though smaller, persist in regions such as Southeast Asia and Europe.
Published in the journal Women and Birth, the study calculated the number of midwives required to perform essential tasks such as providing contraceptive counseling, antenatal care, and support during childbirth. Although there is a noted increase in midwife numbers, the researchers highlighted that the gap between needed and available staff is expected to “persist well into the next decade.” This projection raises concerns about meeting the 2030 target set by global sustainable development goals to reduce maternal mortality and eliminate preventable deaths of newborns and young children.
In response to these alarming statistics, the ICM is calling on governments worldwide to take decisive action. They have launched a global petition to advocate for increased investment in the midwifery profession. “When midwifery is a respected and well-supported profession, more women are motivated to train and stay in the workforce,” af Ugglas emphasized. “That is how countries improve health outcomes and build stronger, more sustainable health systems.”
The pressing need for midwives is not just a workforce issue; it is fundamentally a matter of quality and safety for mothers and their babies. Without immediate and sustained action, the global healthcare community risks failing to protect those who most need care during one of the most vulnerable times in their lives.