Challenges in healthcare systems on both sides of the Atlantic are prompting urgent discussions about surgical efficiency. Hospitals in the United States are cutting back on surgical schedules due to staffing shortages, while the NHS in the United Kingdom reports that more than seven million individuals are waiting for treatment. The impact of these delays is profound, affecting both patient health and hospital finances. According to estimates, inefficiencies in surgical operations cost U.S. hospital systems approximately $32.7 billion each year.
The operating room (OR) is at the center of this crisis. It represents the most resource-intensive area of a hospital, accounting for up to 40% of total hospital costs. Yet, inefficiencies plague these crucial departments. Operations are frequently delayed or cancelled at the last minute, schedules often overrun, and surgical teams spend excessive time resolving conflicts over equipment or scheduling.
A survey of OR leaders revealed that many personnel have left their positions in the past two years primarily due to poor work-life balance, exacerbated by the unpredictable nature of surgical schedules. As healthcare professionals face increased pressure, the consequences extend beyond the hospital walls, resulting in longer wait times and deteriorating health for patients.
Technology as a Solution
Addressing these systemic challenges requires innovative solutions. Dr. Nadine Hachach-Haram, founder and CEO of Proximie, emphasizes the importance of digitizing the OR to enhance performance. By providing real-time visibility into surgical workflows, digital platforms can help teams anticipate problems before they arise, streamline scheduling, and maintain the momentum of surgical procedures.
The integration of technologies such as artificial intelligence, automation, and computer vision can significantly optimize workflows. Data analysis identifies opportunities to reduce downtime between surgeries and improve turnaround times, capitalizing on instances when ORs are underutilized.
Enhancing efficiency not only yields financial benefits but also fosters a more sustainable workload for clinical teams. The U.S. is projected to face a shortage of 30,000 surgeons by 2034, while nurse staffing levels remain below pre-pandemic standards. In the U.K., over three million patients have already exceeded the 18-week NHS target for elective surgeries. The global healthcare workforce crisis is further compounded, with nearly one in five healthcare workers leaving their roles since 2020.
Recruiting new staff alone will not resolve these issues. The working environment must become more manageable for existing employees. Predictability in surgical scheduling is not merely an operational goal; it is essential for staff wellbeing. When teams can rely on timely finishes and reduced delays, both employee satisfaction and patient care improve.
Transforming Operational Efficiency
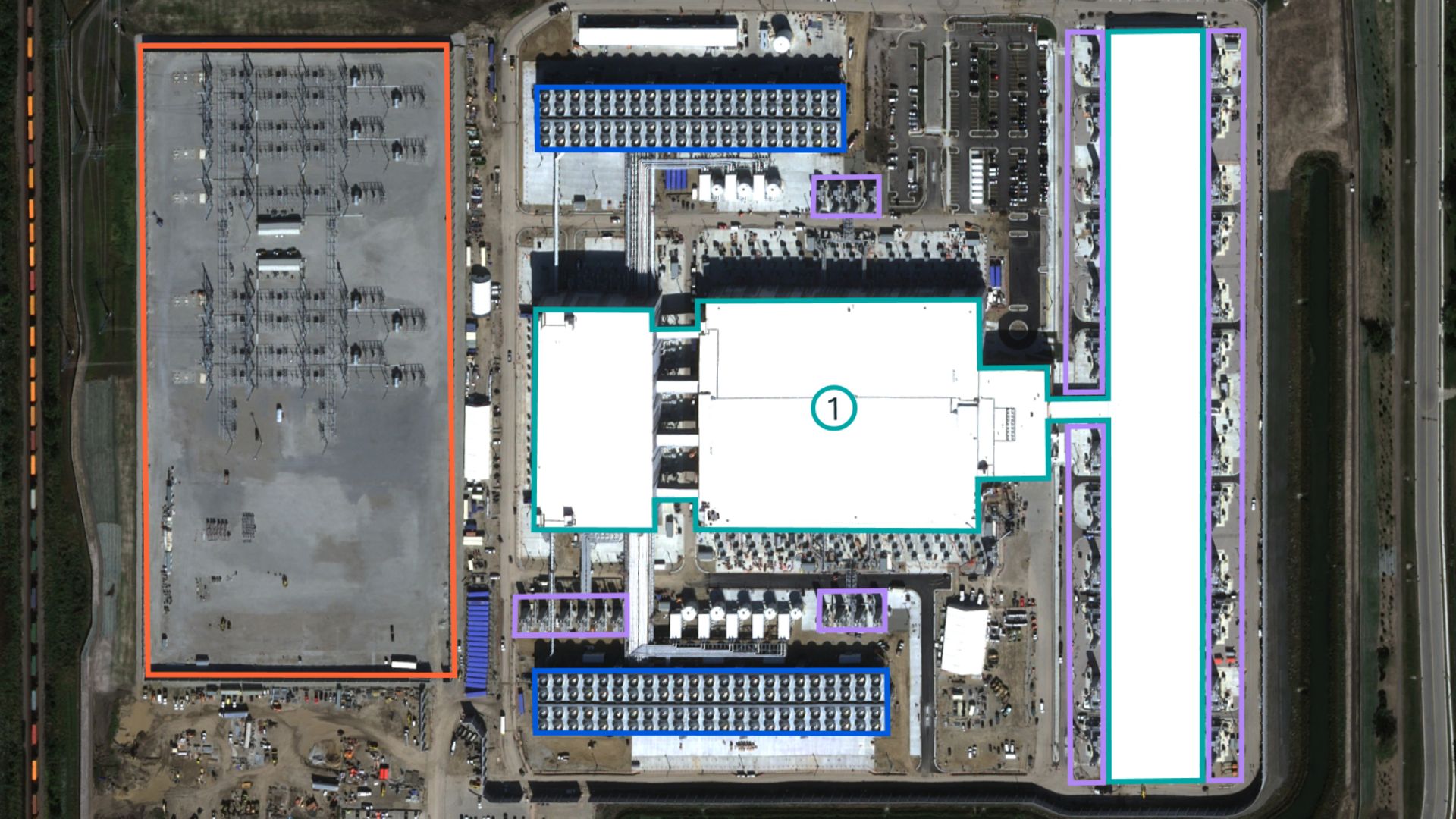
The core of the inefficiency problem lies in the reliance on outdated or incomplete data within ORs, lacking real-time insights into delays and complications. Without accurate, live information, inefficiencies continue unabated, compounding the burden on staff and leading to burnout.
In contrast, digitized OR settings equipped with live data enable clinical teams to track time usage, quickly identify bottlenecks, and seize optimization opportunities. This transition from reactive to proactive management establishes the consistency, safety, and predictability vital for clinicians to succeed.
Recent findings from a major U.S. healthcare provider reveal that nearly 24% of total OR time—averaging 38 minutes per procedure—could be optimized outside of incision time. Capturing this potential could translate into an additional $90 million annually, funds that can be reinvested into staffing, improved processes, and updated equipment.
Healthcare systems are at a critical juncture. The choice is stark: continue with inefficient practices that jeopardize workforce retention or adopt smarter systems that empower clinicians, enhancing the quality of care they provide.
Dr. Nadine Hachach-Haram, a practicing NHS surgeon and clinical entrepreneur, founded Proximie to address these challenges. Her vision for a digitally connected surgical workforce aims to improve access to surgical care globally. Recognized for her contributions, she was awarded the British Empire Medal and has participated in significant initiatives focused on the future of surgery.
As the healthcare industry grapples with its current challenges, the adoption of digital tools in operating rooms could mark a significant step toward achieving both financial sustainability and improved patient outcomes.