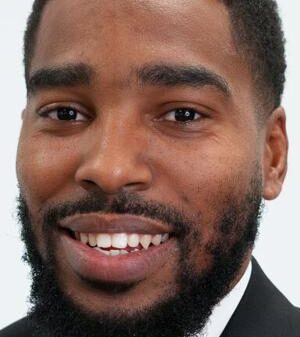
Recent research has established a connection between poor sleep, chronic inflammation, and an increased risk of cognitive decline. A study led by Dr. Howard LeWine, an internist at Brigham and Women’s Hospital and an assistant professor at Harvard Medical School, highlights the significant role that sleep deprivation plays in inflammatory processes that could affect brain health.
Sleep deprivation occurs when individuals do not achieve sufficient quality or quantity of sleep. This condition has been linked to elevated levels of inflammatory markers, such as cytokines, interleukin-6, and C-reactive protein. While other factors like stress, smoking, or obesity can also contribute to inflammation, the evidence suggests that lack of sleep is a critical factor in the inflammatory response.
Understanding the link between sleep and inflammation is essential. Inflammation serves as the body’s natural defense mechanism against disease and injury. However, when it becomes chronic, it can lead to serious health issues, including heart disease, diabetes, strokes, cancers, and notably, Alzheimer’s disease.
Impact of Sleep Deprivation on Inflammation and Brain Health
One theory proposed by researchers is that sleep deprivation affects blood vessel function. During adequate sleep, blood pressure decreases and blood vessels relax. When sleep is limited, this drop in blood pressure does not occur as expected, potentially activating inflammatory processes within blood vessel walls. Additionally, insufficient sleep may disrupt the body’s stress response system, further exacerbating inflammation.
Furthermore, lack of sleep disrupts the brain’s glymphatic system, which is responsible for clearing waste products from the brain. During deep sleep phases, cerebrospinal fluid circulates through the brain, removing beta-amyloid proteins linked to cellular damage. Inadequate sleep impairs this cleansing mechanism, allowing beta-amyloid to accumulate, which in turn leads to more inflammation and cognitive decline.
This creates a detrimental cycle. Accumulated beta-amyloid can hinder deeper, non-REM slow-wave sleep, ultimately affecting memory retention and consolidation. Even one night of poor sleep can elevate beta-amyloid levels, but the cumulative effects of ongoing sleep deprivation are particularly concerning. Over time, this pattern can decrease the structural integrity and function of critical brain regions, such as the thalamus and hippocampus, which are especially vulnerable at the onset of Alzheimer’s disease.
Dr. LeWine emphasizes the importance of addressing sleep issues early. While occasional poor sleep can be compensated for, chronic sleep loss leads to significant brain changes that may have lasting consequences. The findings underscore the need for individuals to prioritize sleep hygiene as part of an overall strategy to maintain cognitive health and reduce the risk of inflammatory diseases.
For more information on health and wellness, visit Harvard Health Publishing at www.health.harvard.edu.