BOSTON — When it comes to measuring weight, BMI is the acronym everyone loves to hate. Health professionals have long used body mass index as a quick screening tool to fast-track certain patients into a “code red” management plan — people whose weight puts them in danger of future health problems. However, a new study suggests that bioelectrical impedance analysis (BIA) may offer a more accurate assessment of health risks.
The issue with BMI is that it calculates health risk by using height and weight, which can lead to misleading results. Muscle and bone weigh more than fat, so BMI can overestimate danger for individuals with a muscular build or larger frame. Conversely, it may underestimate health concerns in older adults and those who have lost muscle, according to the Harvard T.H. Chan School of Public Health in Boston.
Bioelectrical Impedance: A New Approach
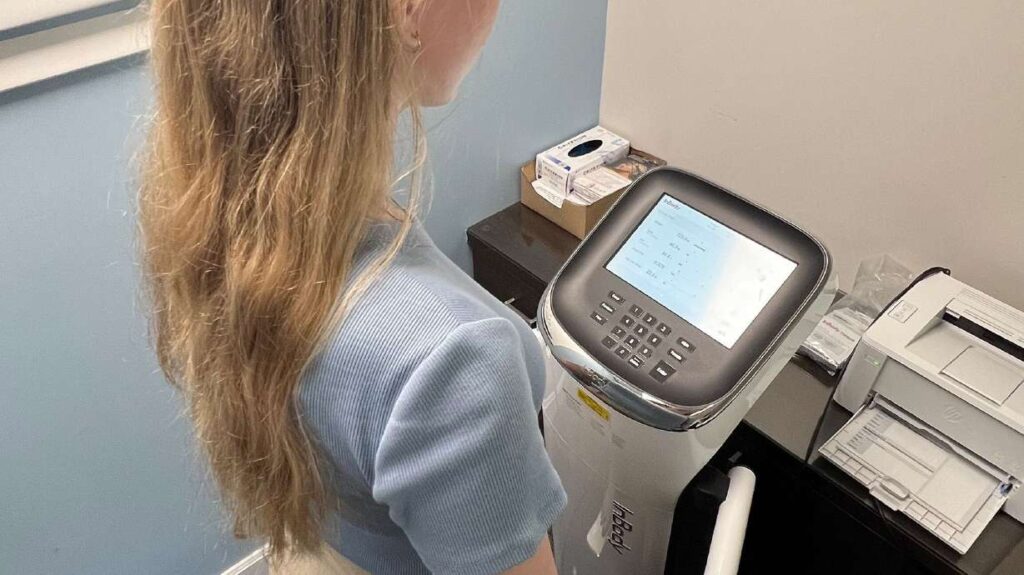
The authors of the new study propose that BIA, which uses undetectable electric currents to measure body fat percentage, lean muscle mass, and water weight, could be a more accurate predictor of future health issues. This technology involves standing on metal plates while holding another metal attachment, allowing a weak electrical current to pass through the body. Different tissues conduct electricity differently, enabling the machine to calculate body composition.
“We found body-fat percentage to be a stronger predictor of 15-year mortality risk in adults between the ages of 20 and 49 than BMI,” said Arch Mainous III, lead author of the study published in the journal Annals of Family Medicine. The study revealed that individuals with high body fat as measured by BIA were 262% more likely to die from heart disease compared to those with a healthy body fat percentage.
The Problem with BMI
BMI is calculated by dividing weight by the square of height. While it is a useful tool on a population level, correlating with chronic diseases such as cancer, heart disease, and diabetes, it falls short at the individual level. For instance, someone who appears thin but has internal fat deposits around major organs might have a normal BMI yet face significant health risks.
“Those people are more likely to have nonalcoholic fatty liver disease, elevated glucose, and blood pressure, and general inflammation,” Mainous explained.
Despite these limitations, BMI remains popular due to its low cost and ease of use. Alternatives like DEXA scans, considered the gold standard for body mass analysis, are expensive and less accessible, costing patients $400 to $500 per scan.
Expert Opinions and Future Implications
Dr. Frank Orlando, senior author of the study, emphasized the potential for early interventions. “Think of the interventions we can do to keep them healthy when we know this early. I think it’s a game-changer for how we should look at body composition,” he said.
While newer versions of BIA are proving accurate, Dr. Andrew Freeman, director of cardiovascular prevention and wellness at National Jewish Health in Denver, cautioned against relying on at-home BIA products due to their susceptibility to hydration levels.
“At-home measurements will only give a ballpark — the clinic-based machines are more precise,” Freeman noted.
Is It Time for a Shift in Medical Practice?
The study analyzed data from 4,252 participants in the National Health and Nutrition Examination Survey (NHANES) and compared it with the National Death Index. The findings indicated that a BMI indicating obesity was not linked to a statistically significant higher risk of death from any cause. In contrast, high body fat measured by bioimpedance analysis was associated with a 78% increased risk of death from any cause.
Orlando argues that these findings make a compelling case for adopting BIA in clinical settings. “Add that to the 262% higher chance of dying from heart disease found by the study, and it’s a no-brainer for doctors to use bioelectrical impedance analysis on patients,” he said.
The announcement comes as healthcare providers continue to seek more effective ways to assess and manage patient health. As research progresses, the medical community may increasingly turn to bioelectrical impedance analysis as a standard practice, potentially transforming how body composition is evaluated in clinical settings.






